The healthcare sector has been through the wringer – scrambling through the pandemic, patching up gaps in digital maturity, and racing to adapt on the fly to new regulations and patient demands.
The pressures are mounting. Staff shortages and clinician burnout rates are at an all-time high. Long admission waiting times and overcrowding are the “default” state. Digitization efforts are undermined by frequent cybercrimes and regulatory scrutiny.
Yet, healthcare leaders aren’t ruffled. Most view ongoing disruptions as a motivator to push ahead with digital transformation initiatives and find new use cases for emerging technologies to address the above challenges.
This post examines key healthcare technology trends, shaping a more agile, patient-centric, and tech-driven industry.
7 Major Healthcare Technology Trends – The Transition to Phygital Care
Medicine has always been science-driven, but today the scales tilt from medical research towards digital technologies and software engineering. In digital-led hospitals, a new model is emerging – phygital care.
About 70% of global healthcare leaders prioritize investments in technology platforms and digital tools, and most expect digital technology use to accelerate in 2025 and beyond. Our team has identified seven main tech areas that will impact care delivery, monitoring, and patient experience.
Personalized Treatments, Powered by AI
Artificial intelligence has been a top technology trend in healthcare for several years, with organizations making progress in their maturity rates. In 2024, adoption rates increased to 35%, according to the American Medical Association (AMA). Encouragingly, 68% of physicians now acknowledge the benefits of AI in healthcare, almost double from the previous year.
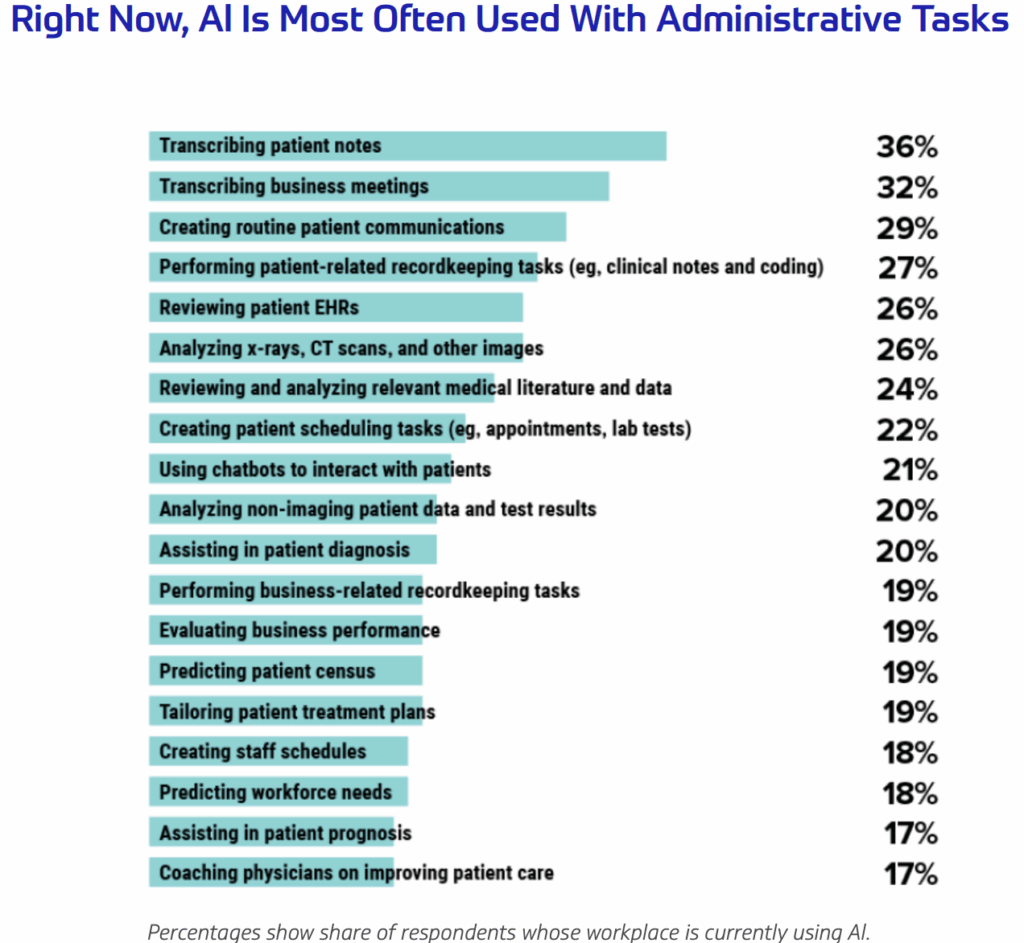
This change in sentiment is largely explained by the top use cases that significantly reduce clinicians' administrative workload:
AI systems can do more than streamline “grunt work.” The algorithm’s ability to process multi-dimensional data – from genomic profiles and medical imaging to lifestyle and EHR data – at scale can enable more precise treatment plans.
In oncology, AI models have successfully matched patients with effective therapies based on tumor genetics. In chronic disease management, predictive models can anticipate flare-ups, prompting early interventions tailored to individual risk factors.
Our team recently helped an American biotech company launch a genomic analysis for multiplex and parallel analysis of biological systems at the cellular, protein, and gene levels, speeding up insights into new treatment methods. Insilico Medicine, in turn, leverages an AI-powered platform to design patient-specific molecules for diseases like idiopathic pulmonary fibrosis. Their drug candidate INS018_055 (the first fully AI-discovered drug) entered phase 2 trials in 2023.
AI can also enable better personalization at the point of care. With limited staff, many hospitals “delegate” routine tasks like patient follow-ups and appointment scheduling to Gen AI agents, trained to provide personalized answers based on the patient’s medical history.
UC San Diego Health recently launched Dr Chatbot – a GPT-4 powered assistant that helps clinicians draft detailed, empathetic messages, based on the patient’s medical history. Such systems improve communication quality and reduce physician burnout, a recent study found.
Combined with another major healthcare technology trend of 2025 – medical IoT – AI systems can enable remote, continuous, and highly-personalized care. Using data from devices, algorithms could suggest medication dose adjustments, recommend behavioral changes, or alert healthcare providers about data anomalies.
Federated AI Learning for Collaborative Research
AI promises breakthroughs in healthcare, but raises operational risks – data breaches, model bias, privacy violations, and more. Federated learning techniques have proved to be a breakthrough for privacy-conscious industries like healthcare, allowing models to be trained on decentralized raw data without moving it.
Instead of exchanging data, federated models dispatch AI models to project participants for on-site training using private datasets. Only the learned insights (model updates) are shared back, aggregated centrally, and used to improve the global model, keeping raw data securely in place. This approach reduces data breach risks and improves compliance with regulations like HIPAA and GDPR. More importantly, it creates a new pane of collaborative clinical research.
The EU’s MELLODDY project proved the viability of this approach. It collected a cross-pharma data set of 2.6 billion experimental data points on 21 million compounds and 40,000 assays, operationalized with a machine learning algorithm. The outcome was several predictive models that significantly outperformed single-partner models in both classification (AUC-PR) and regression (R²) tasks.
Another hospital group has successfully validated a federated learning model for brain tumor segmentation using MRI scans, showing superior glioma boundary detection results.
Other viable federated learning use cases in healthcare include:
- Large-scale genomic research to better understand disease susceptibility and treatment responses
- EHR data analysis to predict patient outcomes, identify risk factors, and improve clinical decision-making
- Multi-institutional collaborations on drug candidate research and clinical trials for accelerated drug discovery
Effectively, federated learning allows healthcare organizations to use collaborators’ data without regulatory risks. Larger, more representative data sets also reduce model bias risks and improve diagnostic accuracy for frequently underrepresented populations or diseases. Lastly, it commoditized access to AI research for smaller institutions, allowing them to contribute data and benefit from insights without investing in their own IT infrastructure.
Remote Patient Monitoring Goes Mainstream
Primary care institutions face a triple squeeze of a rapidly aging population, rising chronic disease rates, and ongoing talent shortages. With millions of patients struggling to access timely care, especially in rural and underserved areas, many providers are being stretched beyond capacity.
Remote patient monitoring (RPM) systems have emerged as a solution. Instead of supervising or admitting patients in person, physicians rely on medical wearables and smart at-home clinical devices for timely, data-driven care. In 2023, 75 million patients used RPMs, and by 2027, 115.5 million will adopt the solutions, Juniper Research estimates.
Several devices have cleared regulatory approvals, including:
- CCN Health platform securely aggregates data from 25+ FDA-approved medical devices to monitor vitals like blood pressure, glucose, and weight.
- Brook developed an AI solution for detecting early signs of congestive heart failure. During a trial at UMass Memorial Health - Harrington, the tool reduced CHF patient readmission rates by 50%.
However, there are untapped product development opportunities for RPM development, specifically in promoting sustainable weight loss with GLP-1s or geriatric care. There’s growing demand for at-home care solutions for post-surgical recovery or chronic disease management.
Early trials show that "hospital-at-home" programs reduce hospital readmissions, lower infection rates, and increase bed capacity. UMass Memorial Health, for example, reduced the number of patient transfers to nursing homes by 80%-90% in the first two years of implementing its at-home elderly care program.
Adoption of RegTech Tools for Compliance
The overlooked flip side of digital transformation in healthcare is growing regulatory compliance. In addition to industry-specific regulations, healthcare providers must comply with relevant technology laws and standards, which increase yearly:
- The EU AI Act sets risk classification levels and compliance requirements for medical AI systems.
- Enhanced FDA/EMA guidelines set stricter cybersecurity requirements for medical devices.
- ISO 42001 established AI management practices for transparency and accountability.
To keep up, many organizations are using RegTech tools for automated tracking of regulatory changes, predictive assessments of compliance statuses and risks, and automation tools to streamline audits, claims processing, and document management.
RLDatix, for example, offers a suite of compliance tools for incident reporting, policy management, credentialing, and regulatory tracking. One of its clients, US Health, reduced serious safety events by 75% post-adoption, thanks to better data integration and proactive risk mitigation.
Radar Healthcare has stellar features for automated compliance workflows (e.g., audits, incident tracking), along with real-time dashboards for risk visibility and status checks against standards like CQC and HIPAA.
New digital solutions help healthcare companies avoid regulatory troubles and improve patient care. Svitla Systems recently deployed an AI-powered opioid data analytics platform that provides insights into prescription practices, compares patient outcomes, and promotes responsible substance usage. The tool is used by over 20 hospitals and 400 ambulatory surgery centers in the US, including Johns Hopkins, Columbia, and Ochsner.
Advancing Cloud Integration in Healthcare
Cloud adoption rates in healthcare have reached over 80%. Many organizations have successfully implemented cloud storage for administrative, archival, research, and patient data and deployed online patient portals for streamlined patient interactions. More mature adopters also leverage the cloud for other e-health services like online prescriptions, telemedicine, remote patient monitoring, and patient billing.
The cloudification of healthcare continues as more cloud service providers (CSPs) launch specialized “health cloud” platforms. AWS HealthLake enables better system interoperability with its Fast Healthcare Interoperability Resources (FHIR) format, allowing standardized, queryable, and interoperable record storage across systems. It also integrates with other AWS tools like Amazon SageMaker and QuickSight for predictive analytics, dashboards, and AI model development using cleaned, labeled data.
SAP Healthcare Cloud, in turn, offers convenient tools for resource planning, procurement, and personalized patient engagement via digital front-door tools. The HIPAA-compliant platform also includes AI tools for clinical decision support, patient risk stratification, and operational forecasting, based on SAP AI Core and AI Foundation services.
Google has also doubled down on its partnerships with healthcare institutions. Already known for its trailblazing solutions for genomics and AI-driven imaging & diagnostics, the company is actively expanding its partnerships with hospitals. Since the start of the year, Google Cloud has partnered with:
- Highmark Health, Hackensack Meridian Health, and Seattle Children’s Hospital on embedding AI agents into clinical workflows for faster data analytics and decision-making.
- Servier, a global pharmaceutical group, plans to use Google Cloud AI across drug R&D, production, and distribution.
- Suki, a medical software vendor, partnered with Google Cloud to power its Suki Assistant with multimodal AI capabilities, including patient summarization and clinical Q&A, streamlining access to critical patient data.
Major CSPs have commoditized access to the latest innovations like generative AI, IoT management, and healthcare APIs, driving interest among healthcare organizations.
Yet, many are held back by legacy systems or concerns over cloud security and compliance. Cloud adoption requires changes to workflows, data usage, and people management. If workloads are simply shifted to the cloud without a strategy, companies could face a larger cloud bill and operational complexities. Consider partnering with a managed cloud development partner for guidance, infrastructure management, and efficient, secure deployment of cloud-first products.
Predictive Analytics for Hospital Operations
Many healthcare institutions continue to run with razor-thin margins, about 5.3% for non-profit hospitals. For-profit hospitals average 14%, although growing labour and supply costs are eroding these gains.
With limited budgets and staff, overcrowding is a significant issue across the UK, the US, and Europe. The Irish Nurses and Midwives Organisation said January 2025 was one of the worst months, with over 13,972 patients waiting for admission.
In the US, where bed occupancy rates exceed 80% in many states, the problem could worsen. By 2035, annual hospitalizations will reach 40 million due to an aging population, while the national occupancy rate will hit 85% by 2032.
To combat the crisis with limited resources, many institutions are turning to predictive analytics systems. With statistical modeling techniques, hospitals can use historical admission data to anticipate demand trends better.
Europe’s largest university hospital, AP-HP, teamed up with Intel to build a cloud-based analytics system that forecasts emergency visits and hospital admissions up to 15 days in advance. By combining EHR data with insights from remote patient monitoring devices, AP-HP can predict trends and individual readmission risks using demographics, comorbidities, lab results, and past treatments.
Across the Atlantic, Johns Hopkins Hospital launched a similar system to identify peak consultation periods and align staffing schedules, ensuring optimal patient coverage and shorter waiting times.
Beyond admission rate forecasting, healthcare big data analytics systems can also enable greater efficiencies in other areas:
- Optimized bed utilization with predicted discharge times and length of stay to improve bed turnover and reduce bottlenecks.
- Staff scheduling – align nurse and physician schedules with projected patient volumes for better coverage and reduced burnout.
- Supply chain optimization using real-time data on demand for various medical supplies, medications, and equipment, and prevent shortages or overstocking.
- Operating room scheduling, based on surgical case durations and cancellation rates to maximize OR utilization and reduce treatment delays.
- Infection control, powered by patient movement and symptom data to anticipate outbreaks and implement timely interventions.
- Patient flow management for smoother transitions between departments (e.g., ER to inpatient care) with real-time admission and discharge predictions.
- Financial planning and reimbursement with modelled cost projections and reimbursement claims based on case complexity and patient outcomes.
All of these use cases have a strong commercial potential and, more importantly, can drive meaningful improvements for patients and clinicians caring for them.
Growing Digital Therapeutics Market
Remote patient monitoring tools can alleviate patient supervision pressures, but they don’t deliver treatments. Digital therapeutics (DTx) – a new generation of software-based interventions – can be used for both remote and in-person interventions.
The first research into using software to treat medical conditions was conducted in the early 1990s, but the state of technology was not yet advanced enough. In 2015, Dr. Cameron Sepah, a clinical professor at UCSF, revived the idea through his research on web-based treatments for chronic conditions, such as diabetes.
Today, the DTx market has hundreds of solutions at different regulatory approval stages.
Countries like Germany, France, and the UK have developed national frameworks for safely using DTx in clinical settings. The US FDA went even further and launched a DTx Center of Excellence to advance research in the area, align regulatory approaches, and support the development of new solutions. In its 2025 Medicare Physician Fee Schedule Proposed Rule, the Centers for Medicare & Medicaid Services has also introduced a potential new reimbursement pathway for DTx products, making treatments more accessible to different patient populations.
To date, digital therapeutics have been successfully used for:
- Chronic disease management: Support for conditions like diabetes, Parkinson’s, and obesity through personalized care plans, symptom tracking, and lifestyle coaching (e.g., Fitterfly, Orbit Health's Neptune).
- Mental health treatment: Clinically validated support for anxiety, depression, PTSD, and ADHD using behavior modification and therapeutic content (e.g., Freespira)
- Substance use disorder: Mobile apps that support sobriety and behavior change, showing higher success rates than standard therapy alone (e.g., re-SET and reSET-O).
- Sleep disorders and insomnia: Prescription DTx programs use CBT and other psychological interventions to treat chronic sleep conditions (e.g., WELT-I).
- Pediatric neurodevelopmental therapy: Gamified DTx solutions to improve attention in children with ADHD (e.g., EndeavorRx).
- Oncology support: Tools to track symptoms, personalize treatment plans, and extend survival rates in cancer patients (e.g., Kaiku Health).
And new products emerge every day. Pfizer released a new application for migraine management that provides personalized insights for symptom management. EpiWatch epilepsy Seizure Management App received FDA 510(k) clearance in early 2025. Evinova, in partnership with Quantum Leap Healthcare, trialled a DTx product for real-time symptom tracking and timely intervention in breast cancer treatment.
With the ongoing harmonization of regulations and the increasing inclusion of DTx into national healthcare reimbursement platforms, there will be an even greater demand among patients in the next couple of years.
Conclusion
As hospitals become increasingly tech-driven, we can expect to see a significant shift from reactive to proactive care models. Rather than treating acute states, physicians will employ predictive data and RPM tools to deliver preventive measures and personalized treatment. AI usage will expand from admin processes into clinical decision support and accelerated medical research as more institutions join efforts with CSPs and leverage federated learning.
Over the next several years, we anticipate that the impacts of new technologies will extend beyond digital transformation to encompass clinical reinvention. Physical hospitals will become just one node in a much larger, intelligent care network that extends into homes, workplaces, and virtual environments.
If you want to be the driving force in this next chapter of healthcare, get in touch with Svitla Systems. We’d be delighted to help you align your digital capabilities with your patient and workforce needs.

![[Blog cover] Top healthcare trends in 2025](https://svitla.com/wp-content/uploads/2025/04/Blog-cover-Top-healthcare-trends-in-2025-936x527.jpg)
![[Blog cover] Top healthcare trends in 2025](https://svitla.com/wp-content/uploads/2024/03/Nataliia-Romanenko-236x236.jpg)
![[Blog cover] Digital transformation technologies in healthcare](https://svitla.com/wp-content/uploads/2025/02/Blog-cover-Digital-transformation-technologies-in-healthcare-560x310.jpg)

![[Blog cover] Benefits of iot in healthcare](https://svitla.com/wp-content/uploads/2025/02/Blog-cover-Benefits-of-iot-in-healthcare-560x310.jpg)